What is hereditary Bowel Cancer?
Bowel cancer (also known as colorectal cancer) is the fourth most common cancer in the UK. Unfortunately, 1 in 18 women (6%) and 1 in 15 men (7%) will develop bowel cancer during their lifetime, with more than 40% being diagnosed over the age of 75.

Most bowel cancer occurs by chance, however 2-5% of bowel cancer is inherited and up to 30% is familial. In some families’ stomach, womb (endometrial or uterine) and ovarian cancer can also be genetically related to bowel cancer. In families where bowel cancer is hereditary it may be possible to find the genetic change (pathogenic variant) which is responsible for the cancers. This allows appropriate cancer screening and risk-reducing options to be offered to the family.
Who is at risk of hereditary Bowel Cancer?
Individuals with hereditary bowel cancer generally show one or more of the following:
- Bowel cancer diagnosed at a young age (before the age of 50)
- Bowel cancer that has screened positive for Lynch syndrome (abnormal IHC/ MSI)
- Several relatives with bowel cancer
- Relatives with bowel cancer and related cancers (such as womb or ovarian cancer)
- Multiple bowel polyps*
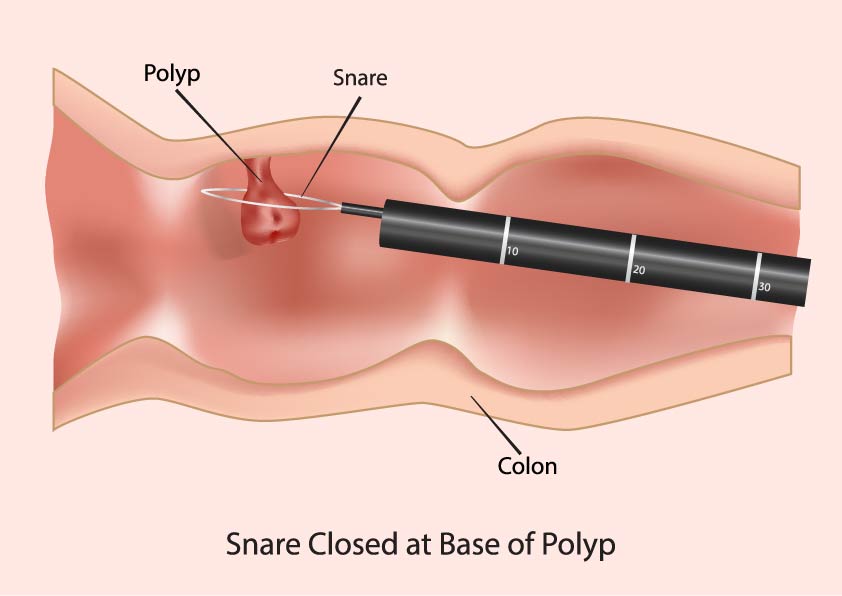
* Cancer usually starts as a benign growth known as a polyp. Not all polyps will become cancerous and they can often be removed during screening.
What are genes?
Genes are the body’s instructions and they determine how the body develops and is maintained. Some genes prevent cancer developing: if there is a pathogenic variant in one of these cancer genes, then the gene doesn’t work correctly and this causes an increased risk of cancer. Pathogenic variants in at least 19 genes can cause an increased risk of bowel cancer and other cancers. However, we know that there are other genes which are also associated with bowel cancer and research is attempting to understand these other genes.

How are pathogenic variants inherited?
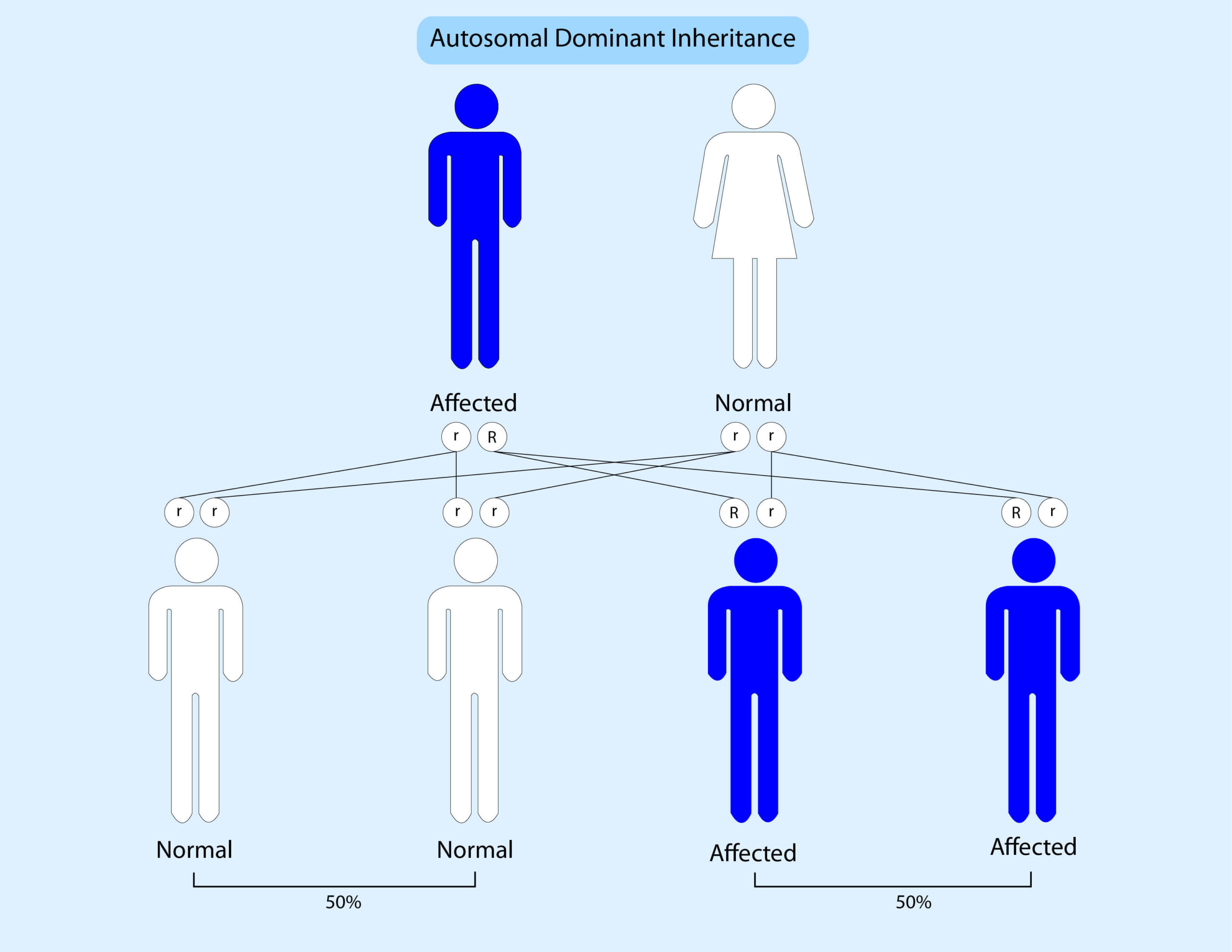
Genes come in pairs; we get one copy from our mother and one copy from our father. Currently most inherited bowel cancer syndromes are inherited in a dominant pattern. This means that if someone has a mutation in one copy of a gene then there is a 50% (1 in 2) chance that they will pass this onto their children. The diagram below shows this:
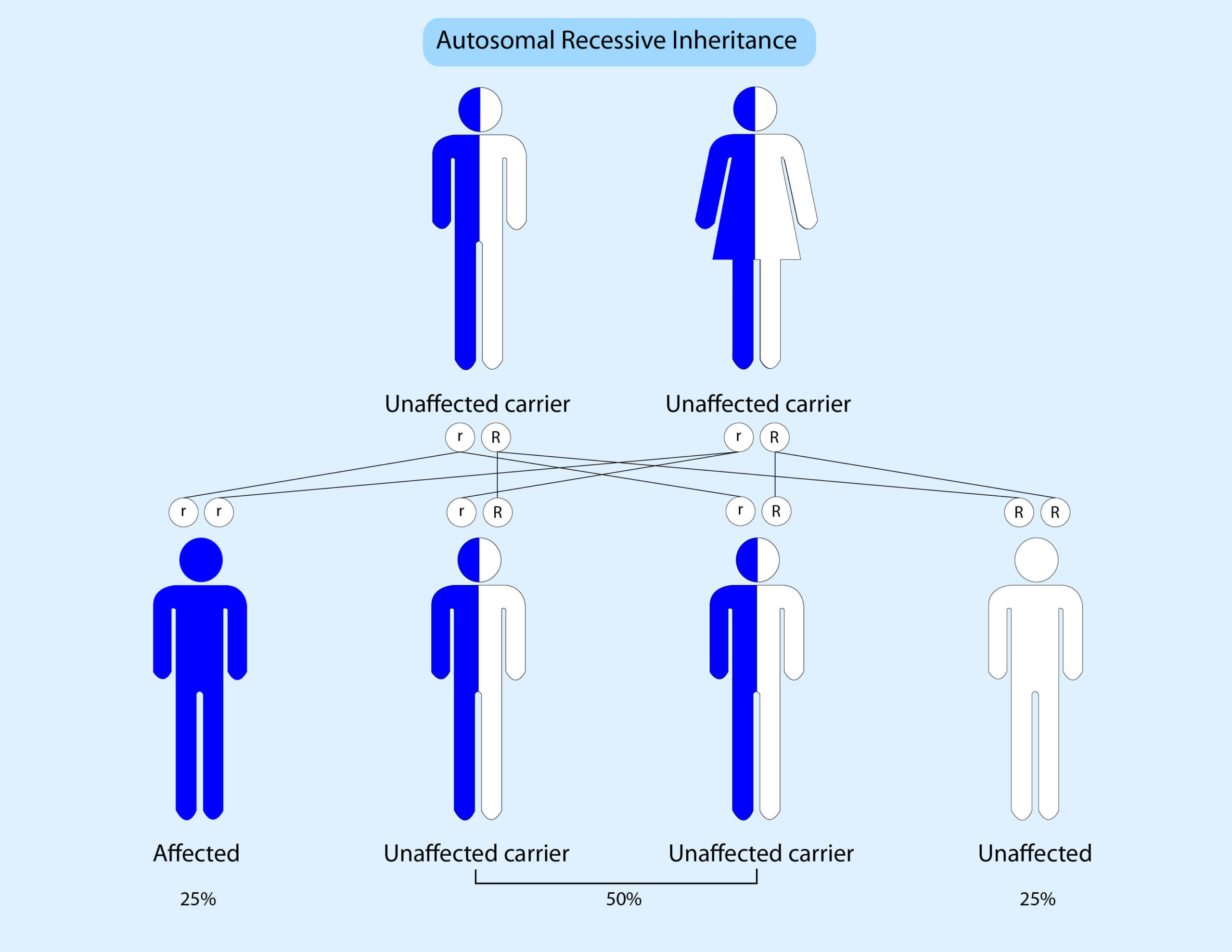
Occasionally an increased risk to bowel cancer can be inherited in an autosomal recessive pattern. This means that someone must inherit a pathogenic variant from their mother AND father to be affected. The diagram below illustrates this:
What genes are tested?
Bowel Cancer Genetic testing looks at 19 specific genes which cause an increased risk of bowel cancer. These genes are explained in more detail below:
How does the test work?
Genetic testing is performed on a blood or saliva sample and it usually takes 4 weeks to obtain the results. The test uses NextGeneration sequencing to examine the code for each of the 19 genes in detail as well as looking for large deletions (missing parts) and duplications (extra parts) of the genes.
It is a comprehensive way to assess a person’s risk for hereditary bowel and associated cancers. However, no test is 100% and it is possible that someone could have a genetic variant which is not detected by this test.
What does it mean if I have a pathogenic variant(s)?
If you have a pathogenic variant in a dominant gene or two variants in a recessive gene, this will explain why you developed bowel cancer and may alter the management of your cancer. You may be advised to consider more extensive surgery and/or different chemotherapy. In addition, you may have an increased risk of other cancers in the future and may need extra cancer screening and/or risk-reducing strategies
It will also be possible to offer predictive testing to other people in your family to see if they also have the mutation.
Conditions which cause inherited bowel cancer
Lynch syndrome (LS): Lynch syndrome is the most common hereditary bowel cancer syndrome and is the cause of approximately 2–3% of all bowel cancer. It is caused by a pathogenic variant in MLH1, MSH2, MSH6, PMS2, EPCAM or possibly MSH3
It has been estimated that in Europe approximately one million people have LS. Cancers which can be increased in Lynch syndrome include: bowel, womb, stomach, ovarian, pancreatic, prostate, urinary tract, liver, kidney and bile duct.
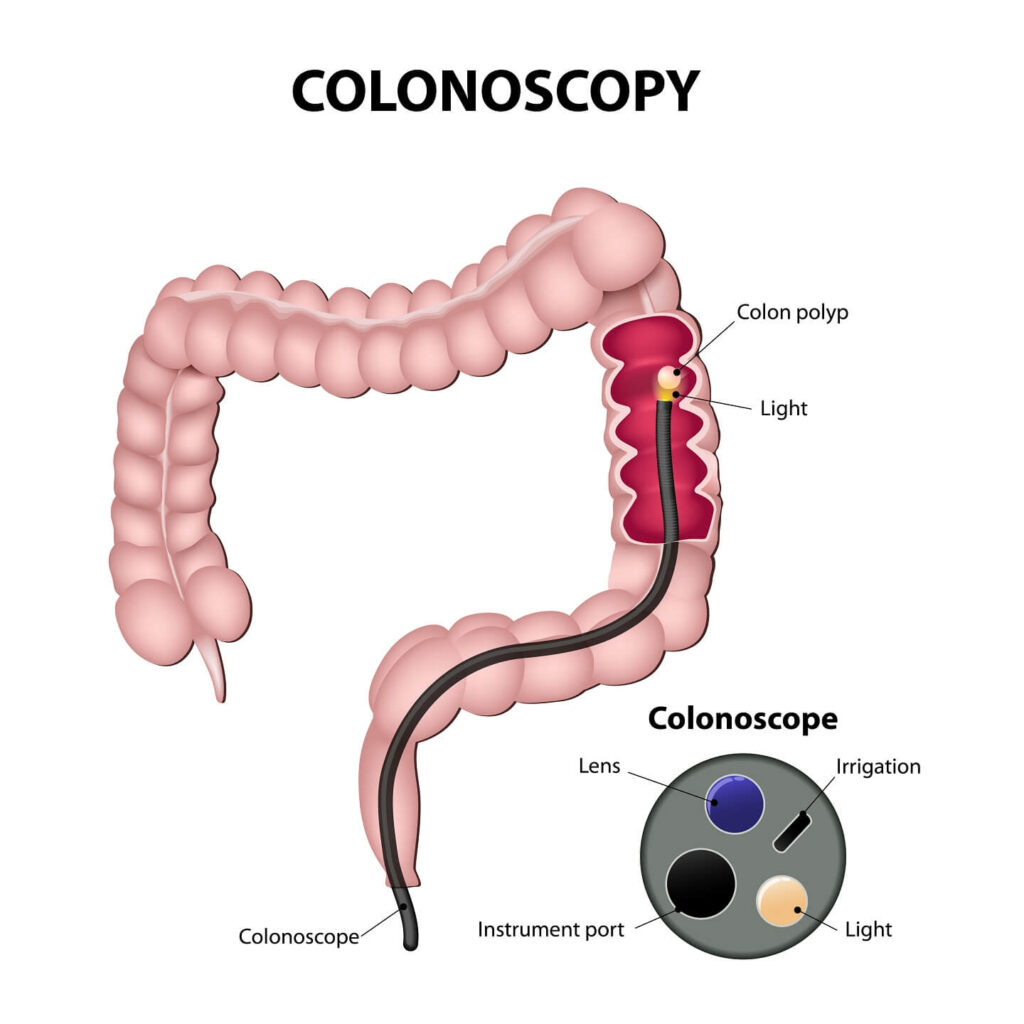
If someone has LS, regular bowel screening with colonoscopy is vital and other risk-reducing strategies will be considered. These strategies include detecting and treating an infection called Helicobacter Pylori as well as taking aspirin, and consideration of risk-reducing surgery.
NICE recommends that all womb and bowel cancer should be screened for Lynch syndrome using either immunohistochemistry (IHC) or microsatellite instability (MSI) testing on the tumour. A further test known as MLH1 methylation or BRAF may also be needed. If the tumour testing screens positive, then further testing on a blood/saliva sample is recommended. NHS hospitals are gradually rolling out these recommendations and therefore these tests may be performed on your/or your relative’s tumour.
Familial Adenomatous Polyposis (FAP) and Attenuated Familial Adenomatous Polyposis (AFAP): FAP and AFAP are inherited conditions which cause multiple bowel polyps (over 100 in classical FAP), as well as a significantly increased risk of bowel, small bowel and other cancers. These conditions are rare: approximately 2-3 people in 100 000 will have FAP. However, about 25% of people with FAP will have a new mutation in the APC gene: this means that it occurred for the first time in them and so they usually won’t have a family history of cancer. If someone has FAP, screening can begin in their teens and they usually consider having their bowel and rectum removed. AFAP seems to be milder with people having fewer polyps and usually a later age of onset and would need increased bowel screening.
MUTYH Associated Polyposis (MAP): MAP is unusual in that it is inherited in a recessive pattern. This means that someone must inherit a mutation from their mother AND father to be affected. MAP causes multiple bowel polyps, an increased risk of bowel cancer and possibly other cancers. Someone with MAP would be advised to have regular colonoscopies.
NTH1 Associated Polyposis: Variants in NTH1 are also inherited in a recessive pattern. This means that someone must inherit a mutation from their mother AND father to be affected. NTH1 causes multiple colorectal polyps and an increased risk of colorectal cancer. Increased colonoscopic surveillance is advised.
Juvenile Polyposis syndrome (JPS): Juvenile polyposis causes many polyps in the bowel and most people will develop some polyps by the age of 20. As well as an increased risk of bowel cancer JPS also increases the risk of stomach cancer and possibly other cancers. Colonoscopy and endoscopy screening will be recommended. 22% of people with SMAD4 mutations will also have haemorrhagic telangiectasia (malformations of the veins).
Peutz Jeghers Syndrome (PJS): PJS causes polyps in the large and small bowel, as well as ovarian tumours and abnormal colouring around the lips in childhood. PJS causes an increased risk of bowel, breast, pancreatic and other cancers. Mammograms, colonoscopies and other cancer screening will be recommended.
PTEN Hamartoma Tumour Syndrome (PHTS)/ Cowden syndrome: Cowden syndrome can cause bowel polyps, benign skin lesions, benign breast disease, autism and other features. Individuals with Cowden syndrome have an increased risk of bowel, breast, kidney, thyroid, and womb cancers as well as a risk of melanoma. Colonoscopy as well as mammograms, renal MRI, skin examination and thyroid ultrasounds will be recommended. Risk reducing surgery may be considered.
Hereditary Mixed Polyposis Syndrome (HMPS): HMPS is a rare condition which has been identified in families of Ashkenazi Jewish ancestry and which causes multiple bowel polyps of different types as well as bowel cancer. Regular colonoscopies are recommended.
Li Fraumeni Syndrome (LFS): Li Fraumeni syndrome is a relatively rare condition which causes a high risk of cancer in childhood and adulthood: approximately 1 in 5000 to 1 in 20000, people will have LFS. Li Fraumeni syndrome causes an increased risk of sarcomas, brain tumours, breast cancer, adrenal cortical carcinomas and other cancers. Individuals with TP53 pathogenic variants have a 50% risk of developing some type of cancer by age 30 and a lifetime risk of up to 90%. Breast screening with MRI will be recommended. Individuals are also advised to avoid radiation as they have an increased radiation sensitivity.
What screening would my relatives need?
When someone has an increased risk of bowel cancer it is usual for them to have colonoscopies. A colonoscopy is when a flexible telescope is inserted into the anus to examine the entire bowel (rectum and colon). If any polyps are found these can usually be removed to prevent them developing into cancer. The frequency of colonoscopy will depend on which gene variant is found.
Screening for other cancers may also be needed and will be discussed if necessary. Aspirin has been shown to lower the risk of bowel cancer in some circumstances and is currently recommended for LS carriers.
Risk-reducing surgery
In some situations, people may wish to consider risk- reducing surgery. This is dependent on the condition. In Lynch syndrome women have an increased risk of womb and ovarian cancer and may therefore consider hysterectomy and removal of the ovaries.
In some conditions, people may also consider colectomy (removal of the colon).
Bowel awareness
It is important for everyone to be bowel aware and inform their doctor if they notice any signs that they are concerned about.
The symptoms of bowel (colorectal) cancer in men and women can include:
- bleeding from the back passage (rectum) or blood in your poo
- a change in your normal bowel habit, such as looser poo, pooing more often or constipation
- a lump that your doctor can feel in your back passage or tummy (abdomen), more commonly on the right side
- a feeling of needing to strain in your back passage (as if you need to poo), even after opening your bowels
- losing weight
- pain in your abdomen or back passage
- tiredness and breathlessness caused by a lower than normal level of red blood cells (anaemia)
Further information and support can be found at:
www.corecharity.org.uk 020 7486 0341
www.researchuk.org 0808 800 4040
www.macmillian.org.uk 0808 808 0000
www.bowelcanceruk.org.uk 0800 8403540
Have a question for us?
Contact us
Don’t hesitate to contact us to find out more about genetic testing and consultations
Genetic Experts UK
Email: [email protected]
Phone: 0333 339 2680
This site is protected by reCAPTCHA and the Privacy Policy and Terms of Service apply.
Copyright © 2021 Genetic Experts UK – All Rights Reserved.
Copyright © 2021 Genetic Experts UK – All Rights Reserved.
Website created by Col-Tech Group

